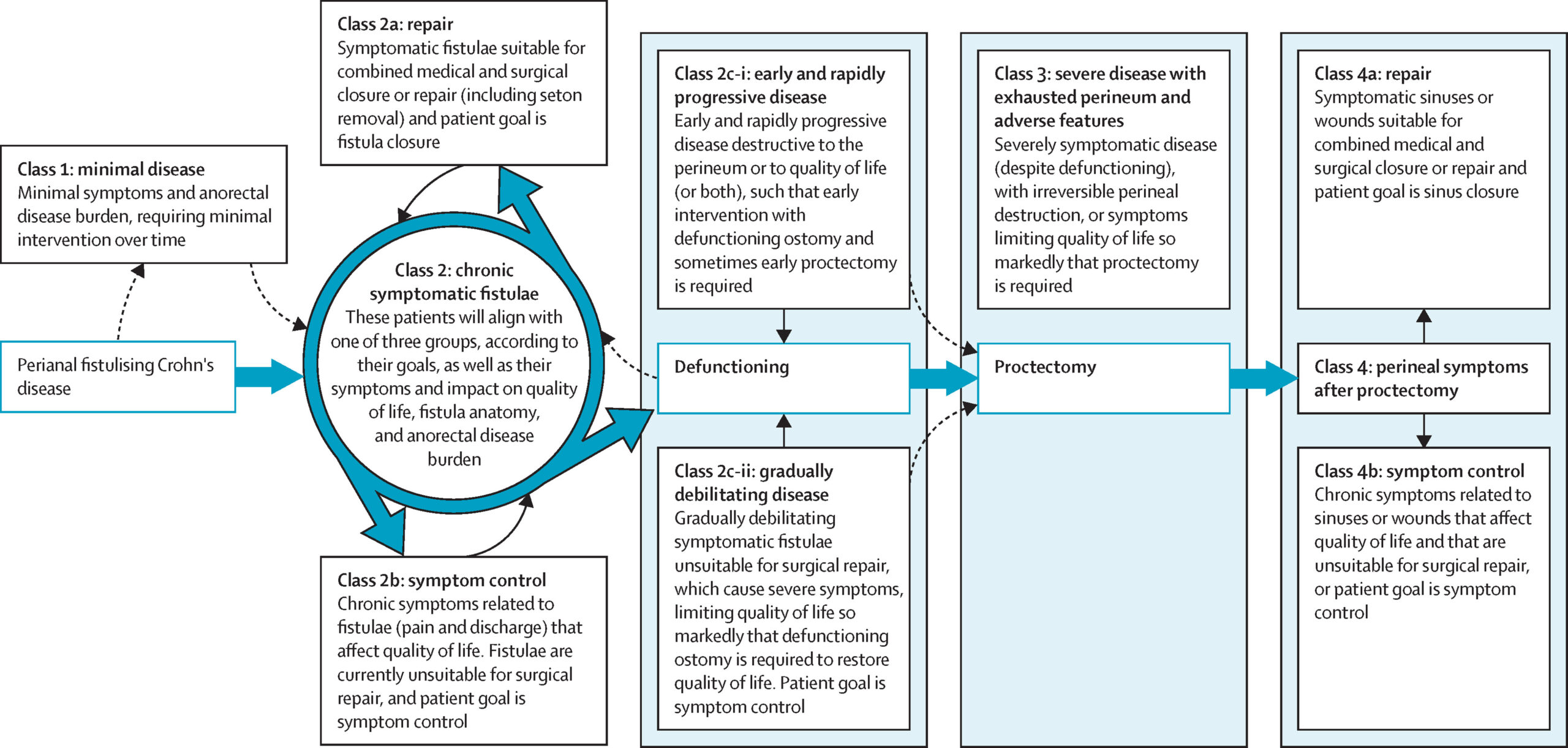
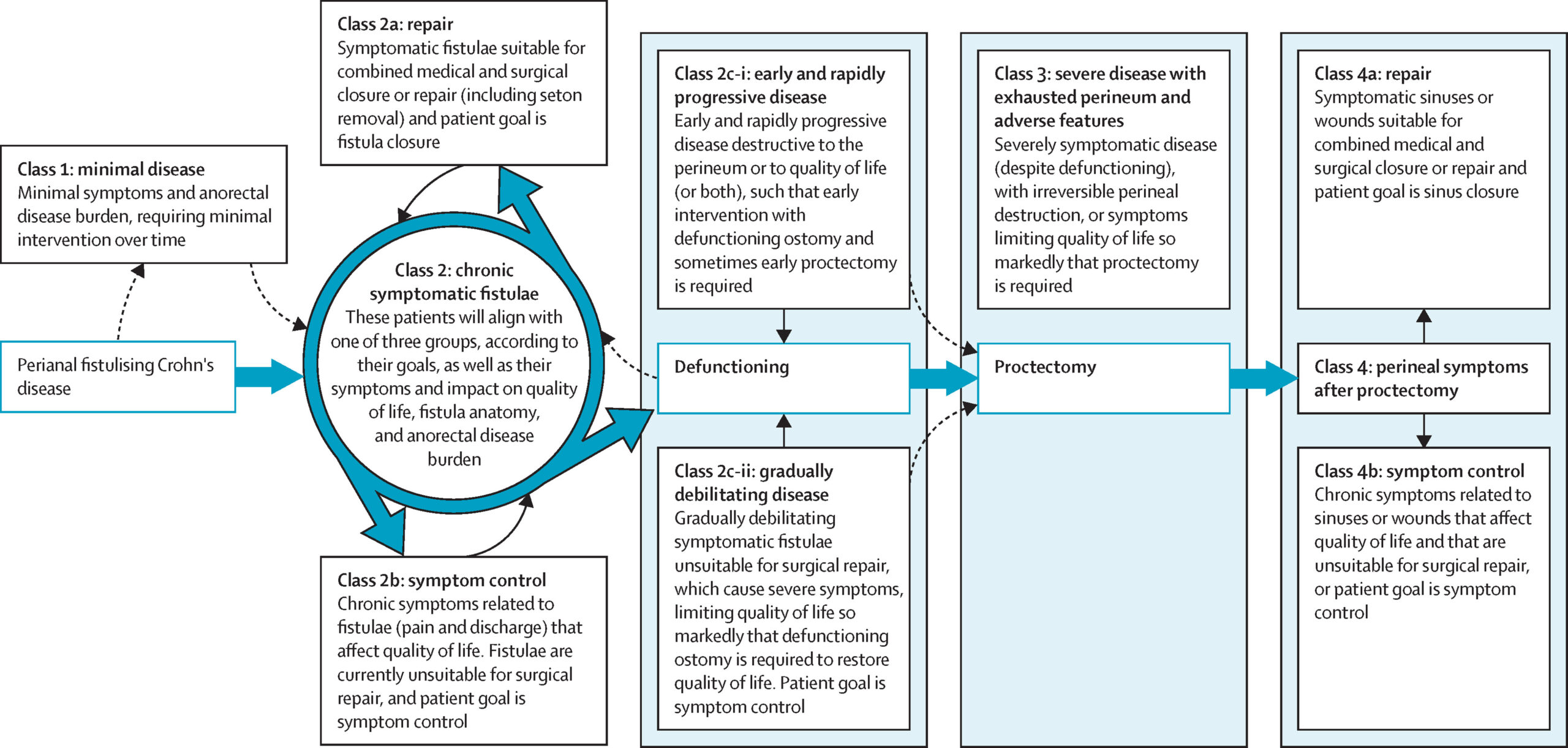
The TOPCLASS perianal fistula classification
Perianal Crohn’s disease can present with ‘fistula’. Fistula are abnormal tunnels, or tracts, that develop between the skin on the outside of the buttock/anal area and the anal canal on the inside (called the ‘rectum’). They can cause unpleasant symptoms like discharge and pain. They are also associated with abscesses.
Fistulas are as individual as the person that has them. No two patients are the same – and different patients will need different (individualised) care plans.
Perianal fistula and Crohn’s disease:
Fistula in Crohn’s disease can be very difficult to treat and can also significantly impact on patient quality of life. Improving the treatment of perianal Crohn’s disease is therefore a research priority in IBD.
The TOpCLASS consortium developed a classification system to help clinicians think about how to treat perianal fistula. It incudes factors such as symptoms, the patient’s own treatment goal, and the severity of the patient’s perianal disease.
The classification system divides patients into different groups:
- Class 1 patients have minimal symptoms and minimal disease burden, which is not affecting their quality of life. The focus in these patients is to prevent progression of their fistula and promote healing with medical therapy. The aim should be to keep the patient remaining well and asymptomatic.
- Class 2 patients have chronic, symptomatic perianal fistula, which are impacting on their quality of life. These patients are divided into three subgroups:
- Subgroup ‘class 2a‘ are patients who would like their fistula to ‘heal’, and whose fistula is felt to be repairable (with surgery) or healable (with medical treatments). The focus of treatment in this group is resolving the fistula (i.e., getting the tunnel to close).
- Subgroup ‘class 2b‘ includes patients who do not want their fistula repaired, or whose fistula is felt to not be immediately repairable or healable. The focus on treatment in this group is improving symptoms and quality of life.
- Subgroup ‘class 2c‘ are patients with progressive disease. These patients either have rapidly worsening, destructive, fistula causing damage to their anal region (class 2c-i) or are suffering from gradually increasing symptoms (class 2c-ii) impacting on quality of life. In both groups, efforts are needed to halt further worsening of their disease and restore quality of life. These patients may also require consideration of a stoma (diverting-ostomy) to achieve this.
- Class 3 are patients who have undergone stoma formation but are still symptomatic from their fistula. Whilst most patients who undergo stoma formation will see an improvement in their symptoms, this is not always the case. Class 3 can be very difficult to manage. Medical and surgical therapies may need to be optimised in this group and, for some patients, removal of the rectum (proctectomy) may need to be considered to treat their fistula symptoms.
- Class 4 are patients who have undergone proctectomy but are still suffering from issues around their perineum in the form of non-healing wounds and sinus tracts. This group is divided into two subgroups:
- Subgroup ‘class 4a‘ are patients who would like their sinus or wound heal, and whose wound/sinus is felt to be repairable (with surgery) or healable (with medical treatments). The focus of treatment in this group is resolving the wound/sinus.
- Subgroup ‘class 4b’ includes patients who do not want their wound/sinus repaired, or whose wound/sinus is felt to not be immediately repairable or healable. The focus on treatment in this group is improving symptoms and quality of life.